Visual Guide to Fatty Liver Disease
Besides liver damage, the rashes might result from HCV treatment. This happens most frequently when people receive hepatitis medicines through injections. In these cases, the rashes could happen where the injection takes place due to irritation.
Cirrhosis Rash: Is Your Rash Caused By Hepatitis?
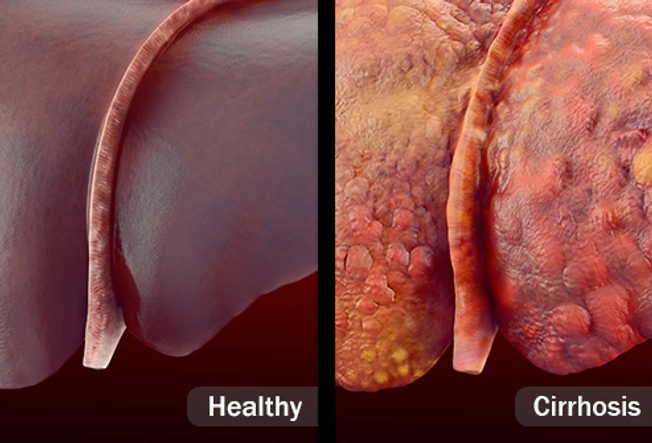
Do you have liver cirrhosis? This is a serious stage of liver disease that involves scar tissue replacing healthy tissue. There are various conditions to watch out for including cirrhosis rash. This serious health condition can cause many symptoms including loss of appetite, leg/ankle swelling, and fatigue. You also might experience rashes. There are various possible causes of this symptom so it’s critical to know the possible causes. This will help to treat it effectively and help manage the disease effectively. In fact, late stages of liver cirrhosis can include mental ones including forgetfulness and confusion. Skin conditions are another type of common symptoms related to liver cirrhosis.
Some symptoms of cirrhosis are linked to other health issues like hepatitis. These conditions can cause several other conditions like rashes. These symptoms can make it tougher to deal with liver cirrhosis. It’s critical to know the real cause of the symptoms so you can deal with them effectively. Skin rashes can be caused by several factors including the hepatitis C virus (HCV). In the USA alone over 4 million people have HCV. However, there are many other causes of rashes so it’s critical to know the real cause of the irritated skin.
What Exactly Is Liver Cirrhosis?
This is a late-stage liver disease that’s very serious and develops over a long period of time. In fact, it’s possible to have liver cirrhosis for several years without experiencing any symptoms. This is related to how serious your condition is.
The first stages of the liver disease result in something called “fatty liver.” This involves extra fat in the vital organ. However, over time this condition can develop into more serious stages. The most serious stage is known as live cirrhosis.
It’s important to get treatment for the liver condition to help prevent the symptoms from getting worse. Here are some symptoms of liver cirrhosis’ early stages:
Administrative costs currently make up a major chunk of healthcare spending, especially in America. In fact, healthcare administrative spending accounts for 8% of the GDP in the U.S., or more than $1.485 trillion if looking at 2016 data. The cost of healthcare administration in other nations is just 3% of the GPD, on average, according to healthcare revenue news source RevCycleIntelligence.
| Hair loss | Personality changes |
| Bleeding gums | Changes in urine/stool |
| Itchy skin | Jaundice (yellow skins/eyeballs) |
| Fever | Low sex drive |
| Confusion | Sleep problems |
| Nosebleeds | Muscle cramps |
| Easily bruising | Stomach swelling |
| White nails | Forgetfulness |
These are some of the symptoms you might experience in the first stages of liver cirrhosis. There are some symptoms you should definitely watch out for:
- Sleepiness
- High fever
- Vomiting blood
- Serious stomach pain
- Confusion
- Yellow eyeballs
- Black stools
- Uncontrollable shaking.
Liver cirrhosis is often linked to alcoholism. However, there are also non-alcoholic causes of liver disease/cirrhosis. When a person experiences cirrhosis their liver isn’t functioning properly. The liver has several functions including producing enzymes for food digestion, removing toxins from the blood, and battling infections.
The liver can normally repair itself and make strong scar tissue. However, when there’s a scar tissue buildup the organ is unable to work properly. This results in liver cirrhosis.
It’s important to know the main causes of liver cirrhosis. They include obesity, hepatitis B/C infections, and heavy drinking of alcoholic beverages. There are also other conditions that might boost your risk of cirrhosis. They include:
- Iron buildup
- Immune system diseases
- Medicine reactions
- Diseases linked to sugar-processing
- Infections
- Genetic disorders
- Blocked bile ducts
- Digestion problems
Can Hepatitis Cause Cirrhosis Rashes?
Hepatitis C virus (HCV) is one of the possible causes of liver cirrhosis. HCV is a type of liver-related contagious infection. When it’s not treated it can cause liver failure. The human liver has many important key functions including infection prevention and food digestion.
HCV causes several possible symptoms including skin rashes. It’s important to treat them ASAP. However, it’s worth noting that there are many causes of rashes and some aren’t directly related to HCV. For example, they could be side-effects caused by HCV medicines. The rashes could also be linked to liver damage itself instead of specific conditions like hepatitis.
HCV causes liver swelling. If the liver isn’t working correctly this can greatly affect your body since the vital organ is critical for several body functions. Hepatitis can cause several symptoms including:
- Stomach pain
- Fever
- Serious fatigue
- Yellow skin/eyeballs (Jaundice)
- Changes in urine/stool
Rashes
When the infection continues and worsens there are more serious symptoms, which can include rashes.
One red flag about rashes is it can be a sign of major river damage. Serious liver damage is closest linked to very serious cases. Liver damage can be seen on the skin. Some possible symptoms include:
- Redness
- “ Spider veins”
- Very dry skin
- Itchy spots
There are other symptoms to watch out for. They include continuous bleeding/swelling. The liver is critical for survival so if it becomes majorly damaged your doctor might order you to have a liver transplant.
Brown patches
Besides liver damage, the rashes might result from HCV treatment. This happens most frequently when people receive hepatitis medicines through injections. In these cases, the rashes could happen where the injection takes place due to irritation.
You can treat this condition using options like hydrocortisone cream and cold packs. This can help to reduce discomfort/ itchiness during the healing process of the rash. Rashes in another area could be a sign of a rare reaction to medicines.
Natural Treatments for Cirrhosis/Hep C Rashes
1. Zinc
This might seem like an odd one. People with hepatitis C have lower levels of the mineral. This can affect various health issues like the immune system and liver. Some studies show that zinc might help to deal with various symptoms and even make treatments more effective.
One Japanese study showed that zinc supplements helped people with Hep C. It reduced their risk of liver cancer versus those who didn’t take the supplements. Make sure to talk to your doctor before taking these supplements to avoid “interactions” with other supplements/medicines.
2. Vitamin D
3. Meditation
It can be tough to deal with rashes linked to cirrhosis/hepatitis. You can help to relax your body/brain through medicine. In the hustle and bustle of the modern world, we often think it’s wasted time when we do nothing. However, this is important for reducing stress and boosting focus. There are various methods. It can involve simply clearing your mind for several minutes. You can also take deep breaths and focus on something we do about 23,000 times per day: breathing.
Your doctor can help you. He/She can provide you with info about meditation classes. They’re offered at different places like community centers, local hospitals, and fitness centers.
4. Massage
Massage therapy can help to deal with soft tissues like muscles by rubbing, kneading, and stroking. Keep in mind this won’t directly treat Hep C. However, it can help to deal with fatigue and lower stress. It’s important to locate a trained therapist so you get the best results when dealing with cirrhosis rash.
Visual Guide to Fatty Liver Disease
Fatty liver could be the most common disease you’ve never heard of. At least 1 out of 4 people have it, which is more people than diabetes and arthritis combined. And lots of those who have it may not know they have it — or even what it is. Most times, this liver disease is mild, but it can lead to more serious health problems. Yet you can often control or reverse fatty liver with smart changes to your lifestyle.
What Is It?
2/14
When too much fat builds up in your liver, that’s fatty liver disease. There are two basic types: nonalcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease, also called alcoholic steatohepatitis. Sometimes, the extra fat can trigger changes that stop your liver from working well. Since your liver filters toxins out of your blood, that could make you very sick.
Nonalcoholic Fatty Liver Disease
3/14
The most common type of fatty liver disease is usually harmless. But some people develop a more severe version called nonalcoholic steatohepatitis (NASH). That’s when your liver gets inflamed, which can lead to cirrhosis (scars on the liver that don’t heal) and a greater chance of liver cancer and heart disease. Experts think NASH is about to become the leading reason for liver transplants.
Who Does NAFLD Affect?
4/14
Experts don’t fully understand why some people get it and others don’t. But you’re more likely to if you’re overweight or obese; have diabetes, high cholesterol and triglycerides, high blood pressure, or hepatitis C and other liver infections; or take certain medications, including steroids or drugs for cancer or heart problems. Most people with this type of fatty liver are middle-aged. But the disease can happen to anyone, even kids.
Alcoholic Fatty Liver Disease
5/14
People who drink a lot — more than one drink a day for women and two for men — get this type. Being obese or a woman raises your chances, too. So can problems that you’re born with in your genes. This can be the first stage of more serious problems. If you keep drinking, you could go on to have alcoholic hepatitis, cirrhosis, liver failure, and higher odds of liver cancer.
Symptoms
6/14
Most of the time, there are none. That’s why so many people who have it don’t realize they do. But some people may feel pain or pressure in the middle or right side of their belly, or be very tired. And sometimes, fatty liver and related problems can make you lose your appetite and lose weight.
Diagnosis
7/14
Because it often has no symptoms, doctors can miss fatty liver disease. Typical lab tests may not catch it either.
Special blood tests can check how well your liver works. Your doctor may want to do an ultrasound or CT scan to see how your liver looks. You might need a biopsy: The doctor will use a needle to get a very small sample of your liver to check it for signs of disease.
Treatment
8/14
There are treatments for fatty liver disease that have varying success. They include vitamin E, liraglutide (Saxenda, Victoza), semaglutide (Ozempic, Rybelsus, Wegovy), and pioglitazone (Actos).
But you can make lifestyle changes to control the disease – or even make it go away.
Lose Weight
9/14
Obesity is the main cause of NAFLD. So if you’re heavy, talk with your doctor to come up with a plan to work off some weight based on healthy eating (with fewer calories) and being more active. A pound or two a week is good — lose too fast, and you can actually make fatty liver disease worse. Dropping just 3% to 5% of your body weight can help.
Exercise
10/14
Even if it’s hard for you to exercise enough to help you lose weight, moderate activity — brisk walking for 150 minutes every week — can get rid of some of the fat in your liver.
Don’t Drink
11/14
When you have alcoholic fatty liver disease, the most important thing to do is stop drinking. It may not be easy, but the benefits are big, especially if you catch it early — you may be able to completely reverse the damage. If you think you have a problem with alcohol, talk to your doctor.
Cutting out alcohol can help with nonalcoholic fatty liver disease, too.
Take Care of Your Health
12/14
Get treatment for related medical conditions, like diabetes and high cholesterol. Ask your doctor if you can stop taking medications that might cause fatty liver disease or switch to different ones. See your doctor (or a liver expert, called a hepatologist) regularly to keep on top of any changes you might need to make to your treatment plan over time.
Be Kind to Your Liver
13/14
You may need shots for hepatitis A, hepatitis B, the flu, and pneumococcal disease to protect your liver and keep you healthy. Also, tell your doctor before you start taking any new medicine, vitamin, or supplement. Even over-the-counter drugs can be hard on your liver.
Prevention
14/14
The same healthy habits that treat fatty liver can lower your chances of getting it. Exercise regularly. Eat a nutritious diet, with good-for-you fats and lots of veggies, fruits, and whole grains. Limit your alcohol. Work with your doctor to manage your health, and follow directions for any medication you take.
Here’s a nice bonus: These strategies also help you avoid other problems, like obesity, diabetes, and heart disease.
Show Sources
IMAGES PROVIDED BY:
1) Thinkstock and Science Source
2) Science Source
Journal of Clinical Gastroenterology: “Low Awareness of Nonalcoholic Fatty Liver Disease Among Patients at High Metabolic Risk.”
National Institute of Diabetes and Digestive and Kidney Diseases: “Definition & Facts of NAFLD & NASH,” “Treatment for NAFLD & NASH,” “Diabetes, Heart Disease, and Stroke.”
American Diabetes Association: “Statistics About Diabetes.”
CDC: “Improving the Quality of Life for People With Arthritis, At A Glance 2016.”
Cleveland Clinic: “Fatty Liver Disease.”
Johns Hopkins Medicine: “Nonalcoholic Fatty Liver Disease.”
MedlinePLus: “Fatty Liver Disease.”
FamilyDoctor: “Nonalcoholic Fatty Liver Disease.”
American Liver Foundation: “NAFLD,” “Alcohol-Related Liver Disease.”
World Journal of Gastroenterology: “Liver transplantation and non-alcoholic fatty liver disease.”
JAMA Internal Medicine: “Effects of Moderate and Vigorous Exercise on Nonalcoholic Fatty Liver Disease: A Randomized Clinical Trial.”
Mayo Clinic: “Nonalcoholic fatty liver disease.”