Slideshow: Hip Surgery Recovery Timeline
After the surgery, notify your doctor if you notice any of the following:
Hip Replacement Recovery: Q&A with a Hip Specialist
There are a lot of moving parts when it comes to recovery after surgery, especially a major one such as hip replacement. How should you prepare? What challenges should you expect? Will you need a caregiver?
All of this takes careful planning among your care team, you and your family members. Johns Hopkins orthopaedic surgeon Savya Thakkar, M.D., an expert in minimally invasive and robotic-assisted total joint replacements, answers some common questions and shares tips about hip replacement recovery and rehabilitation.
When can I go home after a hip replacement?
“Most patients can start walking and can go home the day of the surgery,” says Thakkar. Most people don’t need bed rest. In fact, moving your new joint keeps it from becoming stiff.
Pre-tax flexible spending accounts (FSAs) are often touted as the answer to high out-of-pocket medical costs, but many FSAs have “use it or lose it” rules. FSA holders lose $50 to $100 per year on average, CBS News reported, but since you’re allowed to contribute up to $2,650, you could risk losing thousands of dollars if you don’t spend your FSA money in time.
If you have a preexisting condition (a heart or lung condition that needs monitoring), or if no one can give you a ride and help around the house right after the surgery, you might need to spend the night at the hospital. People who had complex surgeries or lack support at home may benefit from starting their recovery in an inpatient rehabilitation unit.
Will I need to use a walker at first?
Your care team, which includes your surgeon, therapists and primary care doctor, will evaluate the need for any assistive devices. To reduce falls, you might need a cane or a walker if you feel unbalanced walking on your own, but it’s generally not necessary to keep weight off the hip that went through surgery.
When will my hip incision heal?
“The incisions for a hip replacement surgery nowadays are very small and are closed up with absorbable sutures,” explains Thakkar. The incision is covered with a dressing and takes about six weeks to heal. During this time, it’s OK to shower, but to reduce the risk of infection, bathing and swimming should be put off until the wound fully heals.
How soon does rehabilitation therapy start after the hip surgery?
“Patients will have physical therapy before the hip replacement surgery, and then work with a physical therapist right after the surgery to reinforce exercises before they go home,” says Thakkar. Rehabilitation will continue a few days after the surgery, with visits with physical and occupational therapists two to three times per week, as well as home exercises.
Rehabilitation begins with getting used to regular movements and practicing daily activities, like getting out of bed or a chair, and progresses to practicing more difficult tasks, such as climbing stairs and getting in or out of the car.
Muscle strength plays a big role in being able to perform these and other tasks. This is why resistance training of hip muscles and knee muscles in the legs is a major component of rehabilitation.
Hip and Knee Replacement at Johns Hopkins
The Johns Hopkins Hip and Knee Replacement program features a team of orthopaedic specialists highly skilled in joint replacement procedures. Our team will guide you through every step, from presurgical education to postsurgical care and physical therapy. Our goal is to return you to your desired level of activity as soon as possible.
What is considered a “normal” amount of pain after a hip replacement surgery?
Some swelling and initial pain at the joint are normal after hip replacement. To help reduce pain:
- Take time to rest between therapy sessions.
- Ice the leg and the incision site.
- Take anti-inflammatory medications, after consulting with your doctor, to help with these symptoms.
“Keeping the leg elevated above the heart when you lay down can also help the swelling to recede,” advises Thakkar.
It’s important to pay attention to your pain levels. If you feel like you are consistently at a 6 or more on a 1–10 pain scale, mention it to your doctor, because it could be a sign of infection or another complication. As you continue physical therapy, your pain levels should slowly decrease to about 1 or 2 in 12 weeks after the hip replacement.
How long does it take to recover after a hip replacement?
“On average, hip replacement recovery can take around two to four weeks, but everyone is different,” says Thakkar. It depends on a few factors, including how active you were before your surgery, your age, nutrition, preexisting conditions, and other health and lifestyle factors.
“Achieving a certain level of activity before you have the surgery can help you bounce back more quickly,” shares Thakkar. “We use a regimen called prerehabilitation, or prehab, to help patients get in a physical shape that will set them up for a successful recovery.”
Preparing for Hip Replacement Surgery | Q&A with Savya Thakkar, M.D.
Savya Thakkar, a hip and knee replacement specialist, talks about which conditions may require a hip replacement and what to expect before and after the surgery.
How soon can I return to regular activities after a hip replacement?
The goal of physical therapy is to get you back to your normal life, whether it’s going to work, playing with kids, or engaging in your favorite sport or hobby. Depending on the amount of physical activity a task requires, the amount of time it will take to be able to perform that task differs.
- Driving. If you had surgery on your right hip, it may take up to a month to be able to drive safely again. If it was your left hip, then you might be back in the driver’s seat in one or two weeks. Start in a parking lot and slowly move to rural roads, working your way up to the highway. Taking medications that may impair your coordination, such as opioids, might delay how soon you can go back to driving.
- Work. If you have a desk job with minimal activity, you can return to work in about two weeks. If your job requires heavy lifting or is otherwise tough on the hips, it is recommended to take off about six weeks to recover.
- Sports. For sports with minimal activity, such as golf, you can return when you feel comfortable. For high impact contact sports you should wait about six weeks to get back in the game. Before getting into a pool, you should also wait about six weeks until the incision completely heals.
- Sexual Activity. You can return to sexual activity whenever you feel comfortable.
What could slow down my recovery?
“As with any surgery, there is some risk of complications during and after a hip replacement, which may include infection at the incision site, bone fractures and hip dislocations,” explains Thakkar. If you notice a fever, drainage from the incision site, difficulty moving your hip or severe pain that is not relieved by your medication, contact your doctor immediately.
Taking rehabilitation at a comfortable pace and avoiding sudden, sharp movements can help prevent dislocations and falls that may delay the recovery.
How long will my hip replacement implant last?
Unlike older implants that were metal, modern hip prosthetics are made of a combination of metal, plastic and ceramic parts, so they are more durable and cause fewer issues. These implants can last 20 to 30 years, and the risk of failure and the need for repeat surgeries is low.
How long after replacing one hip should I wait to replace the other?
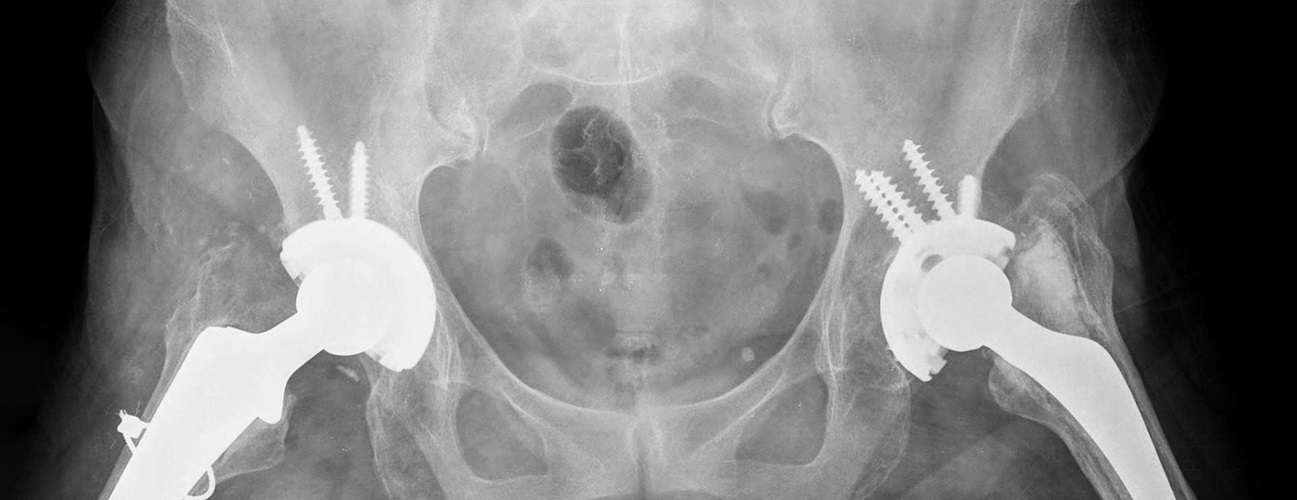
“If you suffer from severe arthritis in both hips, you could get both joints replaced at the same time (double hip replacement). This might actually be safer and lead to quicker recovery in some patients,” says Thakkar.
Having a double hip replacement reduces the risk of many complications that come along with anesthesia. Recovery is actually shorter but may require double the effort, because you would need to strengthen both legs at the same time. It may also be more challenging to get around the house initially, so you might need more support at home.
If you want to have two separate hip replacement surgeries, it is best to wait at least six weeks between the replacements to lower the risk of blood clots.
Find a Doctor
- Degenerative Joint Disease (Osteoarthritis of the Hip)
- Revision Hip Surgery
- Hip Injuries
- Hip Replacement
- Hip Arthroscopy
At Another Johns Hopkins Member Hospital:
- Howard County General Hospital
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
FIND ADDITIONAL TREATMENT CENTERS AT:
- Howard County General Hospital
- Sibley Memorial Hospital
- Suburban Hospital
Slideshow: Hip Surgery Recovery Timeline
Ready for your new hip joint? Check in to the hospital with your bags packed to stay 2-3 days. The operation should take several hours. Afterward, you’ll spend time in a recovery room as you wake up from anesthesia. Once you’re alert, you’ll be moved to your hospital room.
After Surgery
2/9
You’ll probably feel some pain, but you’ll get medicine to help. You’ll likely be taking short, shallow breaths at first because of the anesthesia and medicine, and also because you’re in bed. But it’s important to cough and breathe in deep to clear your lungs. You may have a drainage tube for blood that collects around your hip. Your doctor may give you medicine called blood thinners to prevent clots.
Day After Surgery
3/9
It’s time to get that new hip joint moving. A physical therapist will teach you exercises to strengthen the muscles around it. You will probably sit up on the edge of the bed, stand, and start walking. If your surgery was early in the day and went well, there’s a chance you may even start physical therapy the afternoon of your operation.
1-2 Days After
4/9
You’ll do more exercises and walk with the help of crutches or a walker. As you hurt less, you’ll likely move from IV pain medicine to pills. You should be able to eat normal foods instead of the liquid-only diet you had the first day.
2-3 Days After
5/9
It should be easier to get around now. If you’re doing well, it’s time to go home. Make sure you have help lined up, like rides, shopping, and other errands. You won’t be able to drive for 3-6 weeks. If you need more help, you might check into a rehab center for a few days or have plans for a home health aide to come to your house.
4+ Days After
6/9
Take care of the area around your incision. Don’t get it wet, and skip creams, lotions, and ointments. You can ease pain by using an icepack on the area for 10-15 minutes at a time. Keep the joint moving, and do the exercises you learned at the hospital. You may get visits from a home health nurse or a physical therapist.
10-14 Days
7/9
If you have stitches that don’t dissolve, it’s time to have them removed. Your doctor might suggest you wait another 1-2 days before you shower or get the wound site wet. You should hurt much less now and may no longer need pain medication.
3-6 Weeks
8/9
You should be able to do most of your normal light activities. But you may still have a little bit of discomfort or soreness afterward, especially by the end of the day. Six weeks after surgery, you should be able to drive again.
10-12 weeks
9/9
At this point, you should start to feel like yourself again. Most of your pain is likely gone. Your swelling should have eased. Moving will be easier, and you can probably do most of your regular day-to-day activities, whether it’s gardening, dancing, or taking long walks. You and your new hip will continue to have follow-up visits with your doctor for the first year after surgery.
Show Sources
IMAGES PROVIDED BY:
(1) RNHRD NHS Trust / The Image Bank
(2) iStock / 360
(3) Brand X Pictures
(4) Vstock
(5) iStock / 360
(6) iStock / 360
(7) iStock / 360
(8) Mark Edward Atkinson/Tracey Lee – Blend Images
(9) Pali Rao / E+
American Academy of Orthopaedic Surgeons: “Total Hip Replacement.”
Claudette Lajam, MD, orthopedic surgeon, NYU Langone Medical Center; assistant professor of orthopedics, Hospital for Joint Diseases-New York University School of Medicine.
National Institute of Arthritis and Musculoskeletal and Skin Diseases: “Questions and Answers About Hip Replacement.”
Charles Nelson, MD, chief, joint replacement service, Penn Orthopaedics; associate professor of orthopaedic surgery, Hospital of the University of Pennsylvania.
UCLA Orthopedic Surgery: “Planning for Your Hip Replacement Surgery.”
University of California San Francisco: “Recovering from Hip Replacement Surgery.”
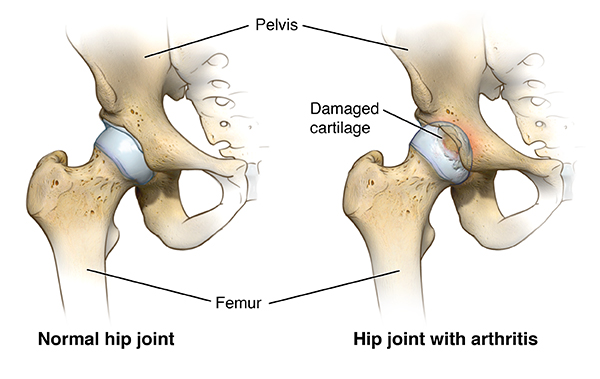
Hip Replacement Surgery
Hip replacement, also called hip arthroplasty, is a surgical procedure to address hip pain. The surgery replaces parts of the hip joint with artificial implants. The hip joint consists of a ball (at the top of the femur, also known as the thigh bone) and a socket (in the pelvis, also known as the hip bone). Hip replacement surgery includes replacement of one or both parts. The goal of the procedure is to allow you to resume daily activities and exercise with less pain.
Who can benefit from a hip replacement?
Your doctor may recommend hip replacement if you have significant pain, inflammation and damage to your hip joint due to conditions such as:
- Osteoarthritis (most common)
- Rheumatoid arthritis
- Osteonecrosis (avascular necrosis)
- Injury such as hip fracture
- Tumor in the hip joint
How do you know if you need a hip replacement?
When your quality of life suffers due to hip pain, it may be time for hip replacement. Signs of declining quality of life include:
- Inability to get restful sleep because of pain
- Difficulty doing simple tasks such as getting dressed or climbing stairs
- Inability to fully participate in the activities you enjoy
At first, your doctor may recommend other treatments such as medicine for pain or inflammation, walking aids, joint injections and physical therapy. If these measures do not relieve pain and stiffness, hip replacement surgery may be necessary to restore function and improve quality of life.
Types of Hip Replacement Surgery
Several factors help determine the type of hip replacement you may need. Your doctor will consider each of the following when planning your care.
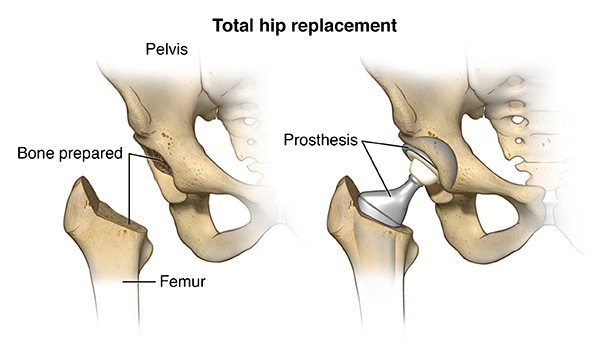
Total and Partial Hip Replacement: Which parts need to be replaced?
During total hip replacement (total hip arthroplasty), both the ball and the socket are replaced. A partial hip replacement only replaces the ball (the head of the femur).
Anterior, Posterior and Lateral Hip Replacement: How will the surgeon access the hip?
An orthopaedic surgeon can access the hip from different angles. Three common ways to access the hip joint are:
- From the front (anterior approach to hip replacement)
- From the side (lateral approach to hip replacement)
- From the back (posterior approach to hip replacement)
Approaches to Hip Replacement Surgery | Dr. Savya Thakkar
Traditional and Minimally Invasive Hip Replacement: How large will the incision be?
Minimally Invasive Hip Replacement
Minimally invasive hip replacement aims to minimize the impact of surgery on healthy tissues, such as muscles and blood vessels. While anterior hip replacement has been marketed as a minimally invasive approach, orthopaedic surgeons nowadays use minimally invasive techniques with all surgical approaches to access the hip. Your surgeon will discuss which approach might offer the best result.
When the surgery is minimally invasive, the surgeon accesses the hip joint though one or two small incisions by moving the muscles aside. This approach may have advantages, such as:
- Lower risk of muscle damage
- Less pain
- Quicker and easier recovery
- Less limping
- Shorter hospital stay
- Lower chance of hip dislocation
Minimally invasive hip replacement is not appropriate for all patients. Your age, weight, fitness level and other factors will help the surgeon decide if you are a good candidate.
Traditional Hip Replacement
A traditional hip replacement includes a single, large incision that helps the surgeon gain access to the hip, usually through the side (lateral approach) or from the back (posterior approach).
Recovery from a traditional hip replacement can take time, because the surgeon needs to cut through or detach some muscles and tendons to get to the joint. (The muscles and tendons are repaired when the hip implants are in place.) You may be at risk for a dislocation until all of your new hip’s supportive structures are healed.
Talk with your orthopaedic hip surgeon to discuss which surgical approach may be best for you.
Discussing the Best Approach With Your Doctor
The surgical approach your doctor will recommend depends on several factors, including how the surgeon will gain access to the hip, the type and style of the implant and how it will be attached, and your age and activity level, and the shape and health of the hip bones. The likelihood of future surgery also figures into the decision, because some surgical approaches and types of implant attachment can make a revision surgery easier or more challenging.
As part of the evaluation for surgery, your orthopaedic surgeon will discuss the options of minimally invasive surgery or traditional hip replacement, as well as how he plans to perform the surgery and what type of implant will be used.
Hip and Knee Replacement at Johns Hopkins
The Johns Hopkins Hip and Knee Replacement program features a team of orthopaedic specialists highly skilled in joint replacement procedures. Our team will guide you through every step, from presurgical education to postsurgical care and physical therapy. Our goal is to return you to your desired level of activity as soon as possible.
Parts of a Hip Replacement Implant (Hip Prosthesis)
The hip replacement implant, also called hip prosthesis, has two parts:
- A ceramic ball attached to a metal stem, which is inserted into the thigh bone (femur) for stability
- A metal cup (typically made of titanium) with an inner plastic layer, which is attached to the socket part of the hip joint (acetabulum) to allow the prosthetic joint to rotate smoothly
In the past, the ball was made of metal as well, but the current standard is ceramic.
Types of Socket Implant Attachment
- Uncemented prosthesis attaches with a porous surface, which allows bone to grow over time and hold it in place.
- Cemented prosthesis attaches with bone cement.
Both uncemented and cemented approaches can work well to secure the implant. As hip replacement techniques have evolved over the years, the cement used has improved, as have methods to encourage natural bone re-growth.
For some hip replacements, the surgeon will combine methods. He or she might prefer to use cement on the femoral stem while using an uncemented attachment on the socket piece that fits into the hip bone.
Can you get both hips replaced at the same time?
Both left and right hips can be replaced during a single surgery. A double hip replacement is also called a bilateral hip replacement. If you are having issues with both hips, your doctor might recommend a double hip replacement if you are in good health and can tolerate a longer surgery and a more challenging recovery.
What happens during a hip replacement surgery?
Hip replacements are performed in a hospital or surgery center. They are often considered outpatient procedures, even though you might need to stay a night or two for observation or to resolve complications.
A typical, uncomplicated total hip replacement surgery has the following steps.
- Once in the operating room, you will get an intravenous (IV) line in your hand or arm. A urinary catheter may be inserted as well.
- You will receive anesthesia, either general (whole body) or below-the-waist (epidural), depending on the recommendation of your anesthesiologist and orthopaedic surgeon.
- The surgeon will place you in an appropriate position to access the hip joint and make an incision. The incision’s location depends on which approach (front, back or side) the surgeon uses.
- The surgeon will remove the head of the femur (the ball part of the joint) and make an opening in the top of the femur. He or she will then insert the stem of the ball prosthesis, with or without cement. The ceramic replacement head will then be attached to the top of the femur implant.
- The surgeon will then remove the damaged cartilage from the acetabulum (the socket part of the joint) and attach the new cup.
- Your surgeon will bend and move your leg to ensure that it functions properly.
- Layers of tissue will be closed with stitches that dissolve. The outermost layer of skin is closed with surgical glue. No stitches will need to be removed after your surgery.
- You will be taken to the recovery room for a couple hours and then transferred to a hospital room. The surgeon will let you know when it is safe to go home, which could be the same day, depending on your condition.
How long does a hip replacement surgery take?
On average, hip replacement surgeries last about two hours. A partial hip replacement might require less time, and a double hip replacement may take longer. Complications during surgery might also extend the surgery time.
You may need imaging, such as an X-ray, immediately after the procedure and during recovery, to confirm that your surgery was successful and that your new hip is healing well.
After a Hip Replacement
Hip replacement recovery starts right away. You will be encouraged to get up and move around as soon as possible after surgery. Patients who don’t have other health conditions can go home as soon as they demonstrate that they can walk, climb stairs, and get in and out of a car.
Some patients might spend time in an inpatient rehabilitation unit to prepare for independent living at home. Whether you go home or to a rehabilitation unit after surgery, you will need physical therapy for several weeks until you regain muscle strength and good range of motion.
The surgeon, physical therapist or occupational therapist can advise you on when you are ready to walk with or without assistance, and how to manage your pain. The provider will discuss your rehabilitation needs, what to expect in the days and weeks ahead, and how to make the most of your recovery. Your motivation and cooperation in completing the physical therapy is critical for an effective recovery process and overall success of the surgery.
While you recover, be sure to:
- Keep the surgical area clean and dry. Your doctor will give you specific bathing instructions.
- Take all medications as directed.
- Keep all the follow-up appointments with your surgeon.
- Attend physical therapy and complete home exercises.
- Resume your normal diet unless otherwise instructed.
- Elevate the leg and use ice to control swelling.
- Do not drive until your doctor says it is safe to do so.
Some fluid might drain from your incision. This is normal during the first few days after surgery. Let your surgeon’s office know right away if you have increased redness, swelling or draining from the incision, high fever, chills or severe pain. Also contact the office if your pain is not improving.
What are the risks of hip replacement surgery?
Most patients do well with hip replacement. As with any surgical procedure, there are some risks during and after a hip replacement:
- Bleeding
- Infection
- Blood clots in the legs or lungs
- Leg length discrepancy
- Injury to nearby nerves
- Fracture
- Continued pain or stiffness
- Dislocation
- Loosening or wearing out of the prosthesis
- Unrelieved joint pain (this may be temporary)
In very, very rare cases of bone surgery, particularly procedures using cement, an embolism (blockage) can occur if fat from the bone marrow enters the bloodstream. A fat embolism can raise the risk of a heart attack or stroke.
There may be other risks depending on your medical condition. Be sure to discuss any concerns with your doctor before the procedure and ask which risks are highest for you.
After the surgery, notify your doctor if you notice any of the following:
- Fever
- Redness, swelling, or bleeding or other drainage from the incision site that doesn’t stop after a few days
- Increased pain around the incision site
- Pain in the lower leg that is unrelated to the incision
- New or increased swelling of the lower leg
Call 911 or go to an emergency room if you experience:
- Chest pain
- Shortness of breath
Revision Hip Replacement Surgery
Your hip implant may wear out or loosen over time. It might also become damaged if you have an injury or dislocation. You may need a revision surgery to replace the damaged parts of the prosthesis. Most hip prostheses last 20 years or longer. You might be able to extend the life of your implant by doing regular low impact exercise, avoiding high impact exercise (such as jogging) and taking precautions to avoid falls.
A rare risk of hip replacement is infection, which can happen if bacteria circulating in the bloodstream get caught in the prosthetic pieces. An infection may require a revision surgery to remove the infected tissues, and a course of antibiotics to kill the bacteria. When the infection is gone, a new prosthetic can be put back in.
If you had a partial hip replacement (only the ball part of the joint), you may need a revision down the road to replace the socket as well.
Find a Doctor
- Degenerative Joint Disease (Osteoarthritis of the Hip)
- Revision Hip Surgery
- Hip Injuries
- Hip Replacement
- Hip Arthroscopy
At Another Johns Hopkins Member Hospital:
- Howard County General Hospital
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
FIND ADDITIONAL TREATMENT CENTERS AT:
- Howard County General Hospital
- Sibley Memorial Hospital
- Suburban Hospital