Recovery From Hysterectomy Week By Week
Abdominal hysterectomy. Most women go home 2-3 days after this surgery, but complete recovery takes from six to eight weeks. During this time, you need to rest at home. You shouldn’t do any tasks until you talk with your doctor about restrictions. Don’t do any lifting for the first two weeks. Walking is encouraged, but no heavy lifting. After 6 weeks, you can get back to your regular activities, including having sex.
What To Expect After A Hysterectomy: Dos, Don’ts, & Tips To Heal
Learning that you need a hysterectomy can bring out all the feelings. On one hand, maybe you’re excited to be getting rid of something in your body causing you pain or bad health. And hey, no more period stress! On the other hand, it’s a big operation, and surgeries can be scary. Some people worry about what the scarring will look like. Knowing what to expect after a hysterectomy can help you calm your nerves and make your recovery as smooth as possible.
Here, Romper speaks with two surgeons who perform hysterectomies day in and day out, and they share exactly what you can expect while recovering from a hysterectomy (including their best tips for healing quickly and comfortably).
Types of hysterectomy
People with uteruses might need a hysterectomy for a wide variety of reasons, like treating fibroids, cancer, or endometriosis, or as part of gender affirmation surgery. Your reason for needing the operation will dictate exactly what kind of hysterectomy you have.
The most common, according to experts, is a total hysterectomy, which removes the uterus and cervix. A partial hysterectomy removes just the uterus, while a radical involves taking out the uterus, cervix, Fallopian tubes, and upper vagina, according to the National Women’s Health Network.
Boris Zhitkov/Moment/Getty Images
What makes healthcare so expensive in America? Rather than mere overuse of medical services, a study published in the Journal of the American Medical Association found that the high cost of medical treatments and procedures is what makes healthcare expenditures twice as costly in the U.S. than in other wealthy countries, The Washington Post
There are also many ways the surgery can be performed. There’s the abdominal hysterectomy, performed through a C-section-like incision about 14 centimeters long just above the pubic hairline. It can be horizontal or vertical.
“In general, patients benefit from minimally invasive hysterectomies, which is anything but the abdominal type,” says Dr. Mary Ellen Wechter, MPH, gynecologist with North Florida Gynecology Specialists and Baptist Health. “The next type is a vaginal hysterectomy, which is the least invasive route. It’s done through the vagina with no incision on the belly. Then, laparoscopic hysterectomies are where there’s an incision in your belly button and about three to four other incisions on the belly and we operate using long, skinny instruments. And a robotic hysterectomy is an advanced technological version of a laparoscopic hysterectomy that allows a more delicate procedure.”
How long does it take for hysterectomy to heal?
Your recovery timeline depends on which type of hysterectomy you’ve had, experts say. “Open surgery typically requires four to six weeks of recovery. Laparoscopic and vaginal surgery typically require one to two weeks of recovery,” says Dr. Louise Perkins King, JD, OB-GYN at Brigham and Women’s Hospital and assistant professor at Harvard Medical School. “Minimally invasive surgery has a wide variety of responses, but typically you’re sent home the same day and are back to work in a maximum of two weeks.”
Shutterstock
And how long can you expect it to take for your incision to heal? The skin may appear healed, but Wechter says the fascia below (the strong tissue layer that holds in your organs) takes about six weeks to repair itself. Lifting or straining before then could lead to a hernia through one of your incisions.
In the first couple of weeks, here’s how Wechter recommends you keep the surgical site clean: “The largest incision is generally in the belly button, and that’s the one that hurts the most and is most at-risk for hernia or infection because it’s deep and dark. You can shower 24 hours after surgery, so I have folks take two Q-tips, rub them on a bar of Dial soap (because it’s antibacterial), and swirl it in the belly button to give it a good wash. Rinse it really well. It doesn’t hurt to put ointment over the incision, like Neosporin or Vaseline even. It seems to help the skin edges migrate together.”
How long does pain last after a hysterectomy?
It’s natural to be nervous about pain post-surgery. If you have an open hysterectomy, you’ll stay in the hospital one or two nights so they can manage your pain levels. King and Wechter agree that patients who have minimally invasive procedures tend not to have much pain at all.
“Pain wise, most people need very little narcotics after surgery,” says Wechter. “The trick is to take pain medication like Tylenol and ibuprofen around the clock on a schedule for the first couple days. Maintaining pain control works way better than chasing pain that’s out of control. Set your timer and take them every six hours to stay on top of it.”
The pain gets better daily, Wechter says. “By the first week people feel pretty darn good. By three weeks, people have almost no pain. By six weeks, people are back to most of their normal activities.”
When can you have sex after hysterectomy?
If your doctor hasn’t told you yet, here’s the bad news: anyone recovering from a hysterectomy is going to have to take a few months’ sabbatical from any bedroom shenanigans. It’s for a good reason though.
“For most people, we have them avoid intercourse for six to 12 weeks,” says Wechter. “Hysterectomies that are complete, meaning we remove the uterus and cervix, have an incision in the vagina. I err on the side of 12 weeks because even if it should be healed, that area can take a lot of pressure during sex.”
Dos and don’ts after hysterectomy
If you don’t have a pal who’s been down this road and can give you some hysterectomy recovery tips, here’s the DL on getting through the next few weeks as comfortably as possible.
Westend61/Getty Images
- Take it easy, tiger. “At least those first three weeks, move kind of like an 80-year-old,” says Wechter. “You can be up and moving around — think like an 80-year-old who’s doing her thing, not a sick 80-year-old – but no bouncing up and down the steps. A lot of fast walking moves the inside tissue of the vagina and can pull on that internal stitch line, and if it’s moving constantly, it doesn’t heal as strongly.”
- Get moving when you’re able. “Remind yourself to get up and move around to keep passing gas and keep from getting a blood clot,” Wechter says.
- Keep your stool softeners handy. “The bowels get paralyzed during surgery with all the other muscles and are a little slow to wake up. Take a stool softener twice a day after surgery and get right on something like Miralax or Dulcolax the morning after to get the bowels moving,” Wechter says.
- Protect your incision. “For larger incisions, we try not to have anything rub on it. Take a maxi pad and turn it soft side in and stick the adhesive side to your underwear so they’re not rubbing the incision,” Wechter says.
- Sit up and stand up carefully. “The main thing is not to use the belly as much as possible and strain those incisions,” Wechter says. “You don’t want to get a hernia. Have someone kind of pull on your hands to help you stand up. When getting out of bed, roll to your side and push up with the opposite arm.”
- If you have pain in unexpected places, don’t panic. “The pelvic floor can sometimes spasm and feel heavy — the muscles that were holding up the pelvic organs are strained and pushed on during surgery. Sitting in a warm bath will help with that,” says Wechter. “Shoulder pains are really common, and they’re actually caused by diaphragm irritation. It’s called referred pain. Maybe there’s gas in the bowel or blood under the diaphragm, and the nerves from the diaphragm are read by the brain as coming from the shoulder, so you’ll feel the irritation there.”
If at any time you notice anything strange about your incision, swelling around your legs, or have a sudden gush of fluid after intercourse, you should call your doctor right away. But rest assured, complications after a hysterectomy are very rare. Just get comfortable on that couch, queue up a new Netflix series, and let your body heal.
Dr. Louise Perkins King, JD, OB-GYN at Brigham and Women’s Hospital and assistant professor at Harvard Medical School
Dr. Mary Ellen Wechter, MPH, gynecologist with North Florida Gynecology Specialists and Baptist Health
Hysterectomy
A hysterectomy is a surgical procedure that removes your uterus. After surgery, you can’t become pregnant and no longer menstruate. Reasons for this surgery include abnormal bleeding, uterine prolapse, fibroids and cancer. Recovery usually takes four to six weeks, depending on the type of surgery you have.
Overview
What is a hysterectomy?
A hysterectomy is the surgical removal of the uterus, and most likely, the cervix. Depending on the reason for the surgery, a hysterectomy may involve removing surrounding organs and tissues, such as the fallopian tubes and ovaries. The uterus is where a fetus grows during pregnancy. Its lining is the blood you shed during your menstrual period. You won’t be able to get pregnant and you won’t get your period after a hysterectomy.
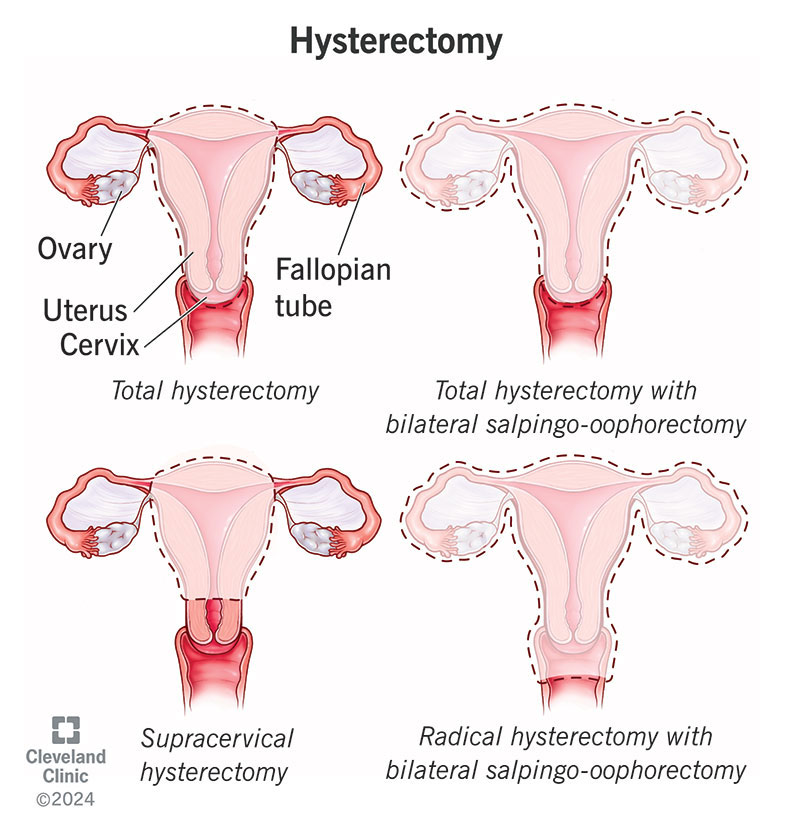
What are the different kinds of hysterectomy?
Your healthcare provider will discuss which type of hysterectomy is needed depending on your condition. This will determine if your fallopian tubes and/or ovaries need to be removed.
- Total hysterectomy: Removing your uterus and cervix, but leaving your ovaries.
- Supracervical hysterectomy: Removing just the upper part of your uterus while leaving your cervix.
- Total hysterectomy with bilateral salpingo-oophorectomy: Removing your uterus, cervix, fallopian tubes (salpingectomy) and ovaries (oophorectomy). If you haven’t experienced menopause, removing your ovaries will start menopausal symptoms.
- Radical hysterectomy with bilateral salpingo-oophorectomy: The removal of your uterus, cervix, fallopian tubes, ovaries, the upper portion of your vagina and some surrounding tissue and lymph nodes. This type of hysterectomy is performed when cancer is involved.
Why is a hysterectomy performed?
Healthcare providers perform hysterectomies to treat:
- Abnormal or heavy vaginal bleeding that isn’t managed by other treatment methods.
- Severe pain with menses that isn’t managed by other treatment methods
- Leiomyomas or uterine fibroids (noncancerous tumors).
- Increased pelvic pain related to your uterus but not managed by other treatments.
- Uterine prolapse (uterus that has “dropped” into your vaginal canal due to weakened support muscles) that can lead to urinary incontinence or difficulty with bowel movements.
- Cervical or uterine cancer or abnormalities that may lead to cancer for cancer prevention.
- Conditions with the lining of your uterus, like hyperplasia, recurrent uterine polyps or adenomyosis.
How common is it to get a hysterectomy?
About 300,000 women get hysterectomies in the United States each year. It’s the second most common surgery performed among women (after Cesarean section).
Procedure Details
How do I prepare for a hysterectomy?
A healthcare provider will explain the procedure in detail, including possible complications and side effects. Talk to them about any concerns you have. You may be asked to provide blood and urine samples.
What happens during a hysterectomy?
Your healthcare provider will determine the type of hysterectomy you need and the best surgical method to perform that procedure. You’ll change into a hospital gown and get hooked up to monitors that track your heart rate. An intravenous (IV) line is placed in a vein in your arm to deliver medications and fluids.
An anesthesiologist will give you either:
- General anesthesia, in which you won’t be awake during the procedure; or
- Regional anesthesia (also called epidural or spinal anesthesia), in which medications are placed near the nerves in your lower back to “block” pain while you stay awake.
There are several different surgical approaches your healthcare provider may use to perform a hysterectomy:
Vaginal hysterectomy
- Your uterus is removed through an incision at the top of your vagina. There isn’t an external incision.
- Dissolvable stitches are placed inside your vagina.
- Most commonly used in cases of uterine prolapse and other nonmalignant (or noncancerous) conditions.
- Fewest complications and fastest recovery (up to four weeks) and considered the preferred approach.
- People often go home on the same day of surgery.
Laparoscopic hysterectomy
- A laparoscope (a thin tube with a video camera on the end) is inserted in your lower abdomen through a small incision in your belly button.
- Surgical tools are inserted through several other small incisions.
- Your uterus can be removed in small pieces through the incisions in your abdomen or through your vagina.
- Some people go home the same day or after one night in the hospital.
- Full recovery is shorter and less painful than an abdominal hysterectomy.
Robotic-assisted laparoscopic hysterectomy
- Your surgeon performs the procedure with the help of a robotic machine.
- A laparoscope is inserted in your abdomen so your pelvic area can be viewed.
- Small, thin surgical tools are inserted through three to five incisions around your belly button. Robotic arms and instruments are controlled by the surgeon.
- The recovery is similar to a laparoscopic hysterectomy.
Abdominal hysterectomy
- Your uterus is removed through a six- to eight-inch-long incision in your abdomen.
- The incision is made either from your belly button to your pubic bone or across the top of your public hairline. The surgeon will use stitches or staples to close the incision.
- Most commonly used when cancer is involved, when the uterus is enlarged or when disease spreads to other pelvic areas.
- It generally requires a longer hospital stay (two or three days) and a longer recovery time.
How long does a hysterectomy procedure last?
The procedure lasts one to three hours. The time can vary depending on the size of your uterus and the need to take down scarring from previous surgeries, as well as if other tissue, such as endometrial tissue, and other organs are being removed with your uterus (like your fallopian tubes or ovaries).
What are the most common side effects of a hysterectomy?
Some of the most common side effects of a hysterectomy are vaginal drainage (which may occur up to six weeks after surgery) and irritation at the incision sites.
If your ovaries were removed at the time of your hysterectomy, you may experience menopausal symptoms such as:
- Hot flashes.
- Vaginal dryness.
- Loss of libido.
- Difficulty sleeping (insomnia).
Your doctor will discuss treatment options to avoid the side effects of menopause mentioned above.
What happens after a hysterectomy?
The amount of time you spend in the hospital following a hysterectomy varies depending on what kind of surgery you had. Your healthcare provider will want to monitor you and ensure there aren’t any signs of complications like blood clots or bleeding. You’ll walk around as soon as possible after your surgery to prevent blood clots in your legs.
If you had an abdominal hysterectomy, you might stay in the hospital for a few days. Vaginal and laparoscopic hysterectomies are less invasive and typically don’t require an overnight stay in the hospital.
Your healthcare provider will go over recovery instructions, including restrictions to your day-to-day activities. Be sure to discuss any concerns you have about your recovery or the procedure.
Care at Cleveland Clinic
- Find Your Ob/Gyn
- Make an Appointment
Risks / Benefits
What are the advantages of having a hysterectomy?
Having a hysterectomy can help you live a more enjoyable life, especially if you have constant pelvic pain or heavy and irregular bleeding. If you’re at a higher risk of uterine cancer, a hysterectomy can lower this risk and potentially be life-saving.
What are the disadvantages of having a hysterectomy?
A hysterectomy is a major surgery with a long recovery. It comes with risks and side effects and is permanent. Depending on the type of surgery you have, you can go into menopause or experience symptoms of menopause. You also won’t be able to become pregnant after the procedure.
What are the complications of a hysterectomy?
As with any surgery, there’s a slight chance that problems may occur, including:
- Blood clots.
- Severe infection.
- Bleeding.
- Bowel blockage.
- Torn internal stitches.
- Urinary tract injury.
- Issues related to anesthesia.
Recovery and Outlook
How long does it take to recover from a hysterectomy?
Most people recover from a hysterectomy in about four to six weeks. Your recovery depends on the type of hysterectomy you had and how the surgery was performed. Recovering from a vaginal and laparoscopic hysterectomy takes less time than recovering from an abdominal hysterectomy.
You should increase your activity gradually and pay attention to how you feel. If anything causes you pain, you should stop. Talk to your healthcare provider about specific instructions for recovering at home, including what medications to take.
What should I know about recovering at home?
Vaginal and laparoscopic recovery take about two to four weeks. It may take up to six weeks to recover from abdominal hysterectomy. Talk to your healthcare provider before going home to make sure you know how to best care for yourself.
Common instructions after a hysterectomy
- You can experience light vaginal bleeding for one to six weeks. Use only a light panty liner or sanitary pad to catch the discharge.
- Don’t lift heavy objects (over 10 pounds) for at least four to six weeks.
- Don’t put anything into your vagina for four to six weeks, or as directed by your healthcare provider.
- Don’t have sex for six weeks after surgery.
- You may take a shower. Wash the incision with soap and water (the stitches don’t have to be removed, as they’ll dissolve in about six weeks). A bandage over the incision isn’t necessary. If surgical strips were used, they should fall off on their own within a week. If staples were used, they’ll need to be removed by your healthcare provider.
- You can drive about two weeks after abdominal surgery or when you’re no longer taking narcotics for pain. If you had a vaginal or laparoscopic hysterectomy, you might begin driving within a few days.
- Resume your exercise routine in four to six weeks, depending on how you feel.
- You can usually go back to work in three to six weeks, depending on what kind of work you do.
How will I feel after a hysterectomy?
Physically
After a hysterectomy, your periods will stop. Occasionally, you may feel bloated and have symptoms similar to when you were menstruating. It’s normal to have light vaginal bleeding or a dark brown discharge for about four to six weeks after surgery.
You may feel discomfort at the incision site for about four weeks, and any redness, bruising or swelling will disappear in four to six weeks. Feeling burning or itching around the incision is normal. You may also experience a numb feeling around the incision and down your leg. This is normal and, if present, usually lasts about two months. It’s normal to have scarring, both internally and externally. Laparoscopic surgeries will cause smaller, less visible scars as opposed to abdominal hysterectomies.
If your ovaries remain, you shouldn’t experience hormone-related effects. If your ovaries were removed with your uterus before menopause, you may experience the symptoms that often occur with menopause, such as hot flashes. Your healthcare provider may prescribe hormone replacement therapy to relieve menopausal symptoms.
People who undergo a subtotal hysterectomy may continue to have a light period for a year after the procedure. This happens because small amounts of the endometrial lining can remain in your cervix, causing light periods.
Emotionally
Emotional reactions to a hysterectomy vary and can depend on how well you were prepared for the surgery, the reason for having it and whether the problem has been treated.
Some may feel a sense of loss, but these emotional reactions are usually temporary. Others may find that a hysterectomy improves their health and well-being and may even be a life-saving operation. Please discuss your emotional concerns with your healthcare provider.
Will my stomach go down after a hysterectomy?
It’s very normal to experience bloating or feeling gassy after a hysterectomy. It can take several weeks for the puffiness and swelling in your belly to go down. Talk to your healthcare provider about ways to reduce your discomfort. Performing certain exercises, applying a warm compress or changing up your diet may help you.
Will I enter menopause after a hysterectomy?
This depends on whether your ovaries were removed. If your ovaries remain after a hysterectomy, you won’t enter menopause right away. If both of your ovaries were removed during the hysterectomy, you might enter menopause immediately.
Do I still need a Pap test if I have had a hysterectomy?
Generally, no, and especially if you’re deemed to be at low risk for developing cervical cancer. You should continue to have a Pap test if you had a hysterectomy because of cancer.
When to Call the Doctor
When should I see my healthcare provider if I had a hysterectomy?
Call your healthcare provider if you have:
- Bright red vaginal bleeding.
- A fever over 100 degrees Fahrenheit (37.77 degrees Celsius).
- Severe nausea or vomiting.
- Difficulty urinating, burning feeling when urinating or frequent urination.
- Increasing amounts of pain.
- Increasing redness, swelling or drainage from your incision.
Additional Details
Does a hysterectomy affect my sex life?
Your sexual function isn’t usually affected by a hysterectomy. If your ovaries were removed with your uterus, this could start symptoms of menopause. Symptoms such as low sex drive and vaginal dryness may occur. Using a water-based lubricant can help with dryness.
Can you still orgasm after a hysterectomy?
Yes, you can still have an orgasm and ejaculate after a hysterectomy. This is because the external organs of your vagina and the pelvic nerves that supply the lower genital tract are still intact after a simple hysterectomy.
Does sex feel different to my partner after a hysterectomy?
No, studies show that sexual pleasure doesn’t change after a hysterectomy. If your ovaries are removed and you have vaginal dryness, using a lubricant can help. In rare cases and when the hysterectomy is performed for cancer or prolapse, the shape of your vaginal canal changes after a hysterectomy. This could lead to pain, especially during penetration.
What fills the empty space after a hysterectomy?
After you have a hysterectomy, your other organs move to fill the space. Your small and large intestines mainly fill the space once occupied by your uterus.
What are alternatives to a hysterectomy?
Your healthcare provider will work with you to develop the best treatment plan for your symptoms or condition. When a hysterectomy isn’t medically necessary, some alternatives to try could be:
- Watching and waiting to see if the condition improves.
- Taking medications such as birth control pills to manage painful periods or abnormal bleeding.
- Burning of the lining of your uterus for heavy bleeding.
- Having procedures to shrink or surgery to remove uterine fibroids.
- Performing exercises for uterine prolapse that help improve the muscles in your uterus.
- Using a pessary to “prop up” your uterus if you have a uterine prolapse.
- Undergoing surgery to treat endometriosis or vaginal bleeding that doesn’t involve removing the entire uterus.
A note from Cleveland Clinic
A hysterectomy can offer relief from many conditions of the uterus, like irregular bleeding or painful periods. Remember, talk openly and honestly with your healthcare provider about your symptoms so they can recommend the best treatment. If you get a hysterectomy, make sure you understand the procedure and how to safely recover from surgery.